Class 12 Biology Chapter 2 – Human Reproduction is a fundamental topic that explores the complex biological processes responsible for the continuation of human life. This chapter provides an in-depth understanding of the male and female reproductive systems, the menstrual cycle, fertilization, pregnancy, and human development from conception to birth. It also covers important concepts such as reproductive health, infertility, and assisted reproductive technologies. Studying this chapter helps students grasp how human reproduction occurs naturally and the scientific advancements that support it. With clear explanations and detailed diagrams, this chapter is essential for Class 12 students preparing for board exams and competitive tests like NEET.
- Human Reproductive System
- Male Reproductive System
- Female Reproductive System
- Spermatogenesis
- Oogenesis
- Differentiation of Gametes
- Menstrual Cycle
- Detailed Explanation of Menstrual Cycle
- Artificial Insemination
- Fertilization
- Pregnancy and Child Birth: From Fertilisation to Birth
Human Reproductive System


Male Reproductive System
- Main organs: testes, vas deferens, prostate gland, penis.
- Testes produce sperm (male gametes).
- Vas deferens transports sperm.
- Prostate gland adds fluid to sperm to form semen.
- Penis delivers semen outside the body during ejaculation.
Female Reproductive System
- Main organs: ovaries, fallopian tubes, uterus, vagina.
- Ovaries produce eggs (ova, female gametes).
- Fallopian tubes transport eggs from ovaries to uterus.
- Fertilization usually occurs in fallopian tubes.
- Uterus supports embryo/fetus development during pregnancy.
- Vagina serves as birth canal and passage for menstrual flow.
Function of Human Reproductive System
- To produce male and female gametes (sperm and egg).
- Facilitate fertilization and formation of zygote.
- Support growth and development of the embryo/fetus.
- Ensure continuation of human species through reproduction.
Male Reproductive System
Primary and Secondary Reproductive Organs of Male: Complete Detailed Notes
1. Primary Reproductive Organs (Gonads)
- Definition:
Primary reproductive organs are those directly involved in the production of gametes (sex cells). In males, the primary reproductive organs are the testes. - Testes (Singular: Testis):
- Location:
Paired oval-shaped organs located in the scrotum, outside the abdominal cavity. The external position in the scrotum helps maintain a temperature about 2–3°C lower than the body temperature, which is essential for sperm production. - Structure:
Each testis contains numerous tightly coiled tubes called seminiferous tubules, where sperm production (spermatogenesis) occurs. The tubules are lined with germinal epithelium containing spermatogenic cells and supportive Sertoli cells. - Functions:
- Spermatogenesis: Production of male gametes (spermatozoa).
- Secretion of Male Sex Hormones: Primarily testosterone.
- Hormones Secreted:
- Testosterone (Androgen):
- Produced by Leydig cells (interstitial cells) found between seminiferous tubules.
- Functions of Testosterone:
- Promotes development of male secondary sexual characteristics (deep voice, facial hair, muscle mass).
- Stimulates spermatogenesis.
- Regulates libido (sexual drive).
- Supports the development and maintenance of male reproductive organs.
- Testosterone (Androgen):
- Location:
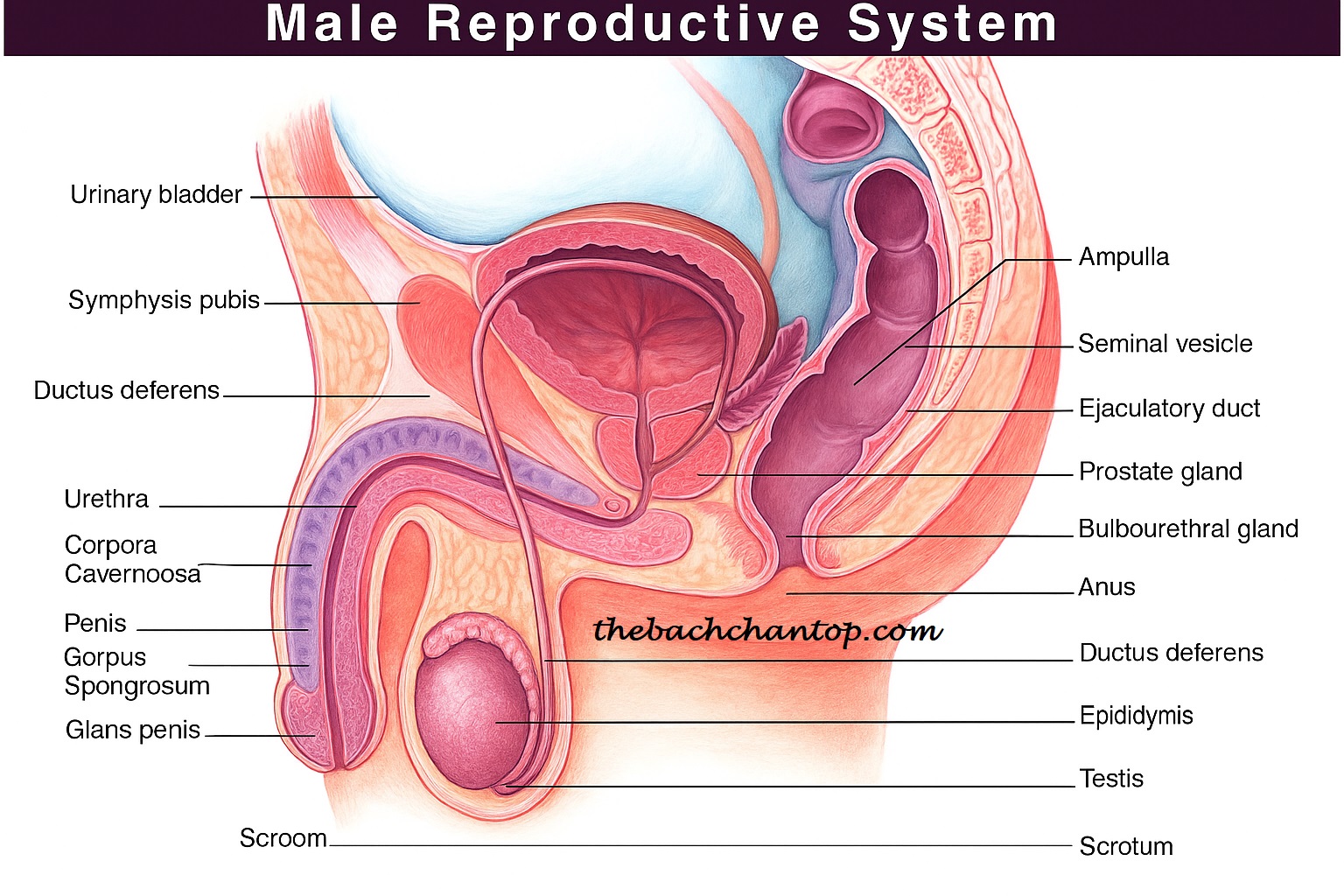
2. Secondary Reproductive Organs
- Definition:
Secondary reproductive organs are those that assist in the storage, nourishment, transport, and delivery of sperm but do not produce gametes themselves. - Major Secondary Reproductive Organs in Male:
- Epididymis:
- Coiled tube attached to the posterior surface of each testis.
- Function: Stores sperm temporarily and allows sperm to mature and gain motility.
- Vas Deferens (Ductus Deferens):
- Muscular tube that transports mature sperm from the epididymis to the urethra during ejaculation.
- Ejaculatory Duct:
- Formed by the union of the vas deferens and the seminal vesicle duct; passes through the prostate gland and opens into the urethra.
- Urethra:
- Conducts semen (and urine) to the exterior through the penis.
- Accessory Glands:
- These glands produce seminal fluid, which nourishes and supports sperm during ejaculation.
- Seminal Vesicles:
- Secrete a viscous, alkaline fluid rich in fructose and prostaglandins.
- Provides energy to sperm and helps neutralize the acidic environment of the female reproductive tract.
- Prostate Gland:
- Secretes a thin, milky, alkaline fluid that also helps sperm motility and viability.
- Bulbourethral Glands (Cowper’s glands):
- Produce a clear, slippery fluid that lubricates the urethra and neutralizes any residual acidity.
- Penis:
- Organ of copulation that delivers sperm into the female reproductive tract.
- Epididymis:
Hormonal Control of Male Reproductive System
- Hypothalamus:
- Secretes Gonadotropin-Releasing Hormone (GnRH) which stimulates the anterior pituitary.
- Anterior Pituitary:
- Secretes two important gonadotropins:
- Luteinizing Hormone (LH):
- Stimulates Leydig cells in testes to produce testosterone.
- Follicle Stimulating Hormone (FSH):
- Stimulates Sertoli cells to support spermatogenesis and produce Androgen Binding Protein (ABP) which concentrates testosterone in seminiferous tubules.
- Luteinizing Hormone (LH):
- Secretes two important gonadotropins:
- Testosterone:
- The main androgen hormone responsible for male secondary sexual characteristics and maintenance of reproductive tissues.
- Inhibin:
- Secreted by Sertoli cells, inhibits FSH secretion by anterior pituitary to regulate spermatogenesis.
Summary Table
| Organ / Hormone | Location / Source | Function(s) |
|---|---|---|
| Testes | Scrotum | Produce sperm and testosterone |
| Seminiferous Tubules | Inside testes | Site of spermatogenesis |
| Leydig Cells | Inside testes | Produce testosterone |
| Epididymis | Behind testes | Store and mature sperm |
| Vas Deferens | From epididymis to urethra | Transport sperm during ejaculation |
| Seminal Vesicles | Near bladder | Produce seminal fluid (fructose, prostaglandins) |
| Prostate Gland | Below bladder | Produce alkaline fluid to aid sperm motility |
| Bulbourethral Glands | Near urethra | Produce lubricating fluid |
| Penis | External organ | Delivers sperm into female reproductive tract |
| GnRH | Hypothalamus | Stimulates LH and FSH release |
| LH | Anterior pituitary | Stimulates testosterone production by Leydig cells |
| FSH | Anterior pituitary | Stimulates spermatogenesis via Sertoli cells |
| Testosterone | Leydig cells | Develops male sex characteristics, supports sperm production |
| Inhibin | Sertoli cells | Regulates FSH secretion |
Hormonal Control
The functions of the male reproductive system are mainly regulated by hormones. The hypothalamus releases GnRH (Gonadotropin Releasing Hormone), which stimulates the pituitary gland to secrete LH (Luteinizing Hormone) and FSH (Follicle Stimulating Hormone).
- LH promotes the production of testosterone (male hormone) in the testes.
- FSH controls sperm production (spermatogenesis).
Onset of Puberty in the Male
Puberty in males usually begins between the ages of 12 and 16. During this period, increased levels of testosterone cause:
- Deepening of the voice.
- Development of muscles.
- Growth of body hair.
- Development of reproductive organs.
- Initiation of sperm production.
Male Sex Act
During sexual arousal, the penis becomes erect. During ejaculation, sperm contained in semen is released outside the body. This process is essential for fertilization.
Disorders of Male Reproductive System
- Infertility: Reduced number or quality of sperm causing difficulty in conception.
- Prostate enlargement: Causes difficulty in urination.
- Testicular cancer: Abnormal growth or lumps in the testes.
- Erectile dysfunction: Difficulty in achieving or maintaining an erection during sexual activity.
Female Reproductive System
Primary and Secondary Reproductive Organs of Female: Detailed Notes (English)
1. Primary Reproductive Organs (Gonads)
- Definition:
Organs that directly produce female gametes (ova) and secrete female sex hormones are called primary reproductive organs.
In females, these are the ovaries.
Ovaries:
- Location:
In the pelvic cavity, one on each side of the uterus. - Structure:
Almond-shaped, each ovary has two main parts:- Cortex: Contains follicles at different stages of development, each housing an ovum.
- Medulla: Contains blood vessels, lymph vessels, and nerves.
- Functions:
- Production of ova (oogenesis).
- Secretion of female sex hormones.
- Hormones:
- Estrogen:
- Secreted by Graafian follicles.
- Functions:
- Development of secondary sexual characteristics (breast development, wider hips, soft voice).
- Thickening of uterine lining (endometrium).
- Regulation of menstrual cycle.
- Progesterone:
- Secreted by the corpus luteum after ovulation.
- Functions:
- Prepares the uterus for implantation.
- Maintains pregnancy.
- Maintains endometrium.
- Inhibin:
- Inhibits FSH secretion to regulate ovum production.
- Relaxin:
- During late pregnancy, relaxes pelvic ligaments and softens the cervix for childbirth.
- Estrogen:

2. Secondary Reproductive Organs
- Definition:
Organs that help in the transport of ova, provide the site for fertilization and fetal development, and facilitate childbirth, but do not produce ova.
Major Secondary Reproductive Organs:
- Oviduct / Fallopian Tube:
- Tube carrying ova from the ovary to the uterus.
- Parts:
- Infundibulum: Funnel-shaped opening near the ovary with fimbriae that capture the ovum.
- Ampulla: Widest part; site of fertilization.
- Isthmus: Narrow part connecting to the uterus.
- Uterus (Womb):
- Pear-shaped muscular organ.
- Layers:
- Endometrium: Inner lining where implantation occurs.
- Myometrium: Middle muscular layer that contracts during labor.
- Perimetrium: Outer covering.
- Functions:
- Site of fetal development.
- Nourishment and protection of the embryo/fetus.
- Cervix:
- Lower narrow portion of the uterus opening into the vagina.
- Vagina:
- Muscular tube serving as the passage for menstrual flow, childbirth, and copulation.
- External Genitalia (Vulva):
- Labia majora: Outer folds of skin protecting the external structures.
- Labia minora: Inner folds protecting the vaginal opening.
- Clitoris: Highly sensitive organ involved in sexual arousal.
- Accessory Glands:
- Bartholin’s glands: Secrete lubricating fluid for the vagina.
- Mammary glands: Produce milk after childbirth for feeding the baby.
Hormonal Control of Female Reproductive System
- Hypothalamus:
- Secretes GnRH (Gonadotropin Releasing Hormone) which stimulates the anterior pituitary.
- Anterior Pituitary:
- FSH (Follicle Stimulating Hormone): Stimulates follicle development in the ovaries.
- LH (Luteinizing Hormone): Triggers ovulation and formation of the corpus luteum.
- Ovaries:
- Secrete estrogen, progesterone, inhibin, and relaxin to regulate reproduction and maintain pregnancy.
Summary Table: Female Reproductive Organs and Hormones
| Organ / Hormone | Location / Source | Function(s) |
|---|---|---|
| Ovaries | Either side of uterus | Produce ova and female sex hormones |
| Follicle | In ovary | Develop ovum, secrete estrogen |
| Corpus luteum | In ovary | Secretes progesterone |
| Fallopian tube | Between ovary and uterus | Transports ovum, site of fertilization |
| Uterus | Pelvic cavity | Site of implantation and fetal development |
| Cervix | Lower part of uterus | Connects uterus to vagina |
| Vagina | Between uterus and outside | Passage for childbirth, menstruation, copulation |
| Bartholin’s glands | Near vaginal opening | Lubrication |
| Mammary glands | In breasts | Milk production |
| FSH | Anterior pituitary | Stimulates follicle growth |
| LH | Anterior pituitary | Causes ovulation and corpus luteum formation |
| Estrogen | Follicles | Secondary sex characteristics, endometrial thickening |
| Progesterone | Corpus luteum | Prepares uterus for pregnancy |
| Inhibin | Ovaries | Inhibits FSH secretion |
| Relaxin | Ovaries | Relaxes pelvic ligaments during childbirth |
Hormonal Control During Puberty
Hormones play a crucial role in the female reproductive system as well. The hypothalamus releases GnRH (Gonadotropin Releasing Hormone), which stimulates the pituitary gland to secrete FSH (Follicle Stimulating Hormone) and LH (Luteinizing Hormone).
- FSH promotes the development of follicles in the ovaries.
- LH controls ovulation (release of the egg).
- Estrogen and progesterone regulate the menstrual cycle and cause the development of secondary sexual characteristics during puberty.
Menopause
Menopause is the stage when a woman’s menstrual cycle permanently stops, usually between the ages of 45 and 55. During this time, hormone production by the ovaries decreases, causing:
- Cessation of menstruation.
- Physical and mental changes such as hot flashes and mood swings.
Disorders of Female Reproductive System
Menstrual Disorders
- Amenorrhea: Absence of menstruation.
- Dysmenorrhea: Painful menstruation.
- Menorrhagia: Excessive menstrual bleeding.
Polycystic Ovary Syndrome (PCOS)
Formation of multiple cysts in the ovaries, hormonal imbalance, and irregular menstrual cycles.
Endometriosis
Growth of the uterine lining (endometrium) outside the uterus, causing pain and sometimes infertility.
Infertility
Problems with ovulation or conception leading to inability to conceive.
Spermatogenesis
Site of Occurrence
Spermatogenesis primarily occurs in the seminiferous tubules of the testes in males.
Process
- Spermatogonia (initial sperm cells) multiply by mitosis.
- They then undergo meiosis to form haploid spermatozoa (mature sperm).
- The process stages are: spermatogonia → primary spermatocyte → secondary spermatocyte → spermatids → mature spermatozoa.
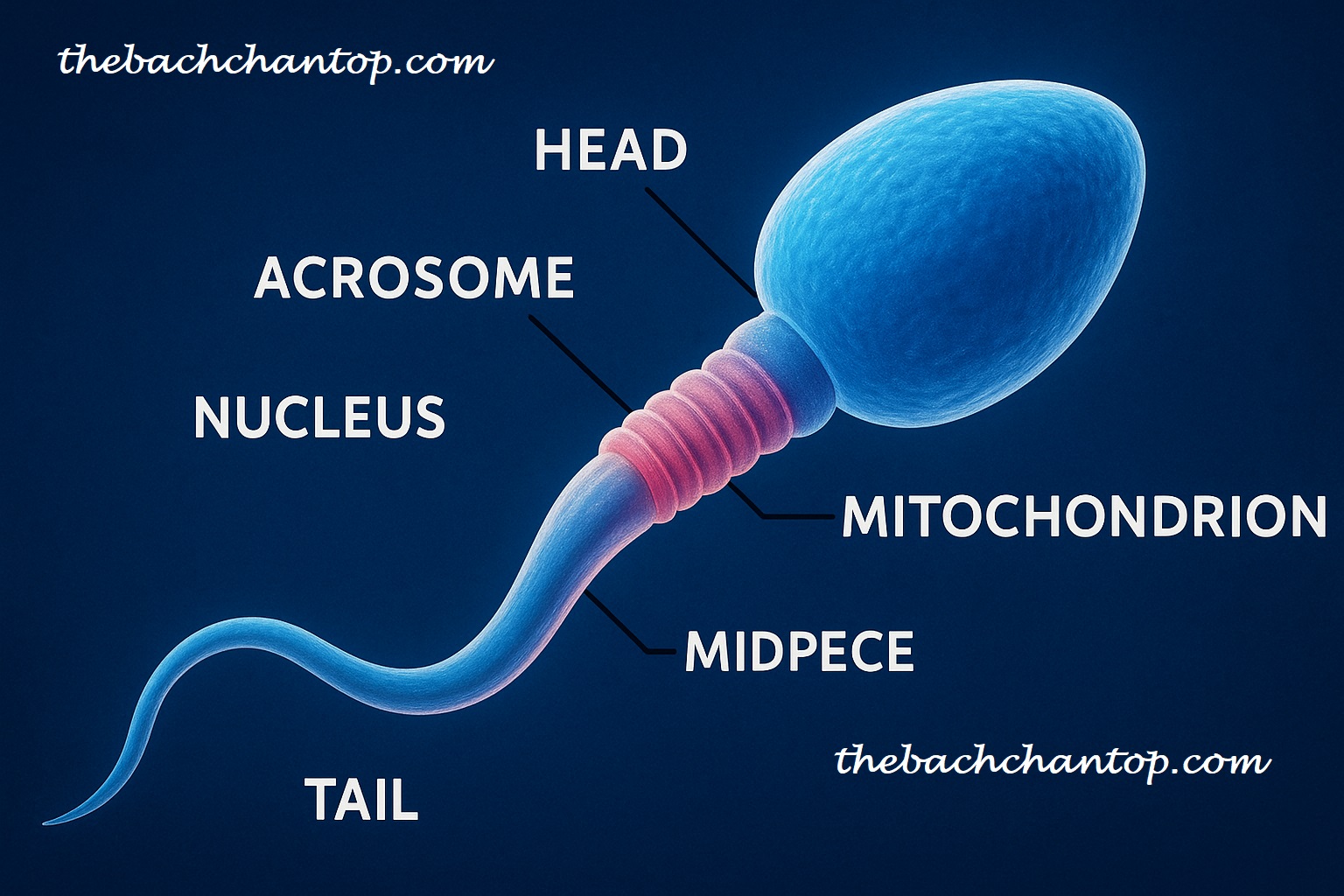
Structure of Spermatozoon
- Head: Contains the nucleus and acrosome, which helps penetrate the egg membrane.
- Mid-piece: Packed with mitochondria to provide energy.
- Tail: Responsible for movement.
Oogenesis
Site of Occurrence
Oogenesis occurs in the ovaries of females.
Process
- Oogonia (initial egg cells) multiply by mitosis.
- Through meiosis, they develop into primary oocytes, then secondary oocytes, and finally mature ova (eggs).
- Meiosis involves unequal cytoplasm division, producing one large ovum and smaller polar bodies.
Structure of Ovum
- Cell membrane
- Cytoplasm containing nutrients
- Nucleus
- Zona pellucida: a thick transparent layer protecting the ovum.

Differentiation of Gametes
Differentiation of Spermatozoon
- Spermatids develop into mature spermatozoa.
- The tail develops to provide motility.
- The acrosome forms to aid fertilization.
Differentiation of Ovum
- Secondary oocyte divides to form the mature ovum.
- Polar bodies form but do not participate in fertilization.
- The ovum contains nutrients to support embryo development.
Menstrual Cycle
- The menstrual cycle is a regular biological process in females lasting about 28 days.
- It involves the buildup of the uterine lining, ovulation (release of egg), and shedding of the lining as menstrual bleeding if fertilization does not occur.
- Main phases:
- Menstrual Phase: Shedding of the old uterine lining.
- Follicular Phase: Development of a new follicle and rebuilding of the uterine lining.
- Ovulation Phase: Release of the egg.
- Luteal Phase: Formation of corpus luteum and hormone secretion.
Detailed Explanation of Menstrual Cycle
What is Menstrual Cycle?
The menstrual cycle is a natural, regular biological process that occurs approximately every 28 days in females. Its purpose is to prepare the body for pregnancy. It involves the thickening and shedding of the uterine lining (endometrium).
Why Does Menstrual Cycle Happen?
Each month, the lining of the uterus thickens to receive a fertilized egg. If fertilization does not occur, this lining breaks down and is expelled from the body as menstrual blood. This process is called menstruation.
The levels of ovarian hormones—estrogen and progesterone—change throughout the cycle and regulate its different phases.
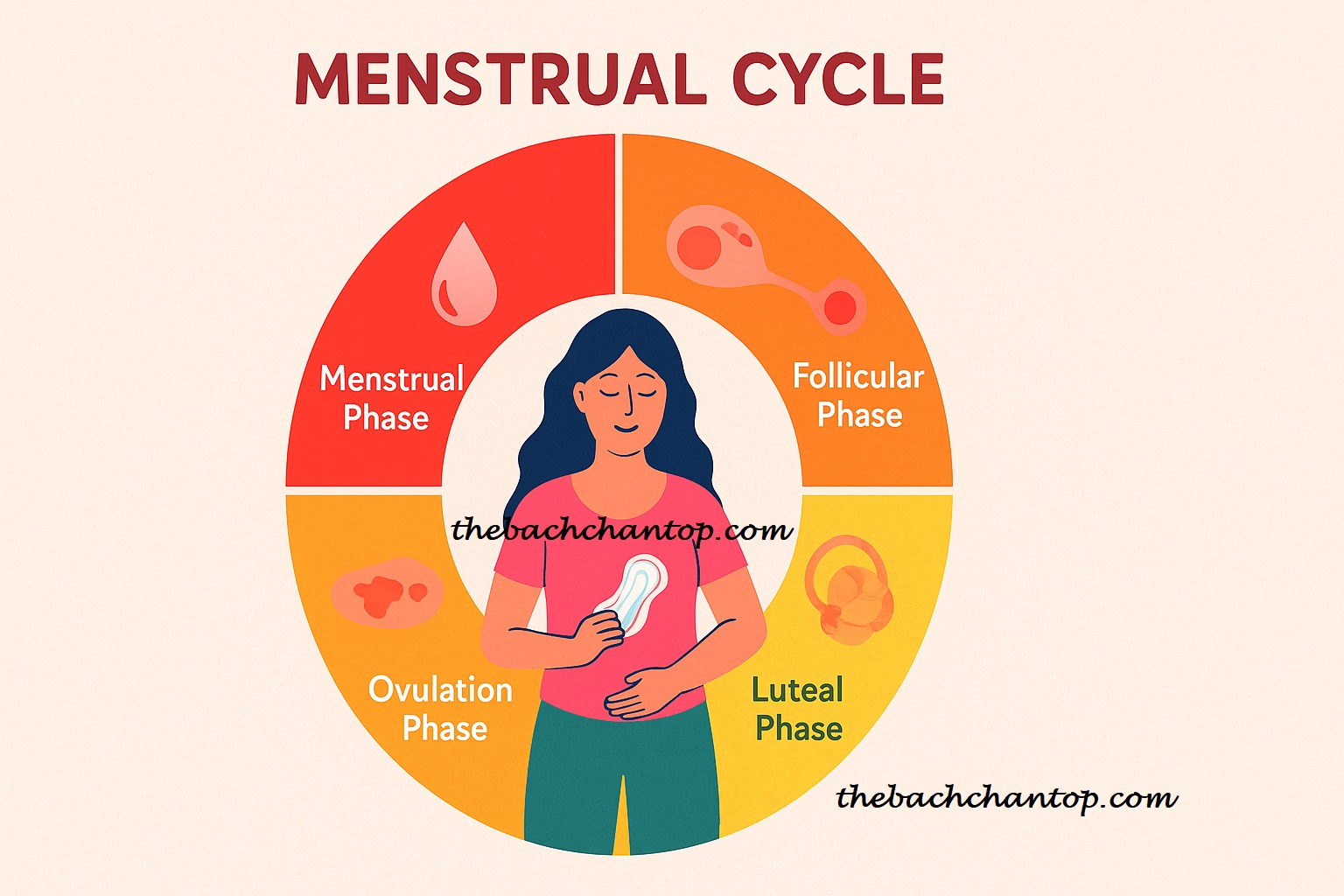
How Does Menstrual Cycle Happen?
The menstrual cycle mainly consists of four phases:
- Menstrual Phase:
- The old uterine lining breaks down and exits the body as menstrual bleeding.
- This usually lasts for 3 to 7 days.
- Follicular Phase:
- The pituitary gland releases FSH (Follicle Stimulating Hormone), which stimulates the development of follicles in the ovaries.
- These follicles release estrogen, which helps rebuild the uterine lining.
- Ovulation Phase:
- A sudden surge in LH (Luteinizing Hormone) causes a mature follicle to release an egg into the fallopian tube.
- This is the most fertile phase of the cycle.
- Luteal Phase:
- The ruptured follicle forms the corpus luteum, which secretes progesterone.
- Progesterone maintains the uterine lining.
- If fertilization does not occur, the corpus luteum breaks down, hormone levels drop, and a new menstrual cycle begins.
Myths vs Facts about Menstrual Cycle in India
Myths
- Women are considered impure during menstruation.
- Women should not enter temples or participate in religious rituals during their periods.
- Women should not cook during menstruation.
- Menstrual bleeding is a sign of illness or weakness.
Facts
- Menstruation is a natural and healthy process; it helps the body cleanse itself.
- Religious beliefs vary, but isolating women due to menstruation has no scientific basis.
- Proper hygiene and nutrition during menstruation are essential.
- Menstrual bleeding is a normal physiological process, not a disease.
Raising awareness about menstruation helps improve women’s health and changes social attitudes.
Artificial Insemination
- An assisted reproductive technology where sperm is directly introduced into the female’s vagina or uterus.
- Used to treat infertility.
Fertilization
Arrival of Spermatozoa
- Millions of sperms enter the female reproductive tract during ejaculation.
Arrival of Egg
- The egg is released from the ovary into the fallopian tube where fertilization occurs.
Capacitation of Sperms
- Sperms undergo biochemical changes in the fallopian tube to become capable of fertilization.
Chemical and Physical Events of Fertilization
- Acrosomal reaction helps sperm penetrate the egg membrane.
- Physical and chemical events lead to the formation of a zygote.
Sex of the Offspring
- Sperms carrying the Y chromosome produce male offspring; those carrying the X chromosome produce female offspring.
Significance of Fertilization
- Fusion of two haploid gametes forms a diploid zygote.
- Ensures genetic variation in offspring.
Species Specificity in Fertilization
- Fertilization occurs only between gametes of the same species due to specific surface molecules on sperm and egg.

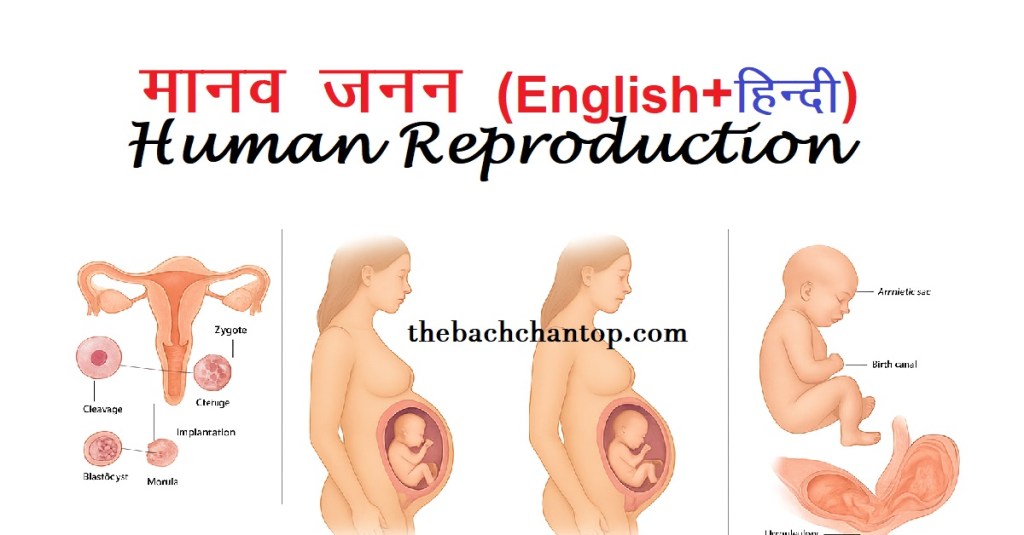
Pregnancy and Child Birth: From Fertilisation to Birth
1. Fertilisation and Early Development
- Fertilisation occurs in the fallopian tube when the sperm cell fuses with the ovum (egg).
- Zygote formation: Single-celled stage formed by union of sperm and egg.
- Cleavage: Zygote undergoes rapid mitotic divisions to form a morula.
- Blastocyst stage: Around day 5–6, the embryo becomes a hollow ball of cells.
- Implantation: Blastocyst embeds into the uterine wall around day 6–7 after fertilisation.
- Hormonal support:
- hCG (Human Chorionic Gonadotropin) is secreted to maintain corpus luteum and progesterone production.
- Progesterone thickens uterine lining and prevents menstruation.
2. First Trimester (Weeks 1–12)
- Key events:
- Formation of placenta and umbilical cord.
- All major organ systems begin to develop (organogenesis).
- Heartbeat detectable by week 6–7 through ultrasound.
- Brain and spinal cord start developing from the neural tube.
- Fetal size: By week 12, fetus is about 6–7 cm long.
- Maternal changes:
- Increased blood volume, morning sickness, fatigue.
- Hormones: Progesterone and estrogen rise steadily.
3. Second Trimester (Weeks 13–27)
- Key events:
- Fetus grows rapidly; bones start to harden.
- Movements (quickening) felt by the mother, usually around week 18–20.
- Skin develops vernix caseosa (protective waxy coating).
- Facial features become distinct; eyelids open.
- External genitalia become distinguishable via ultrasound.
- Placenta is fully functional for nutrient and gas exchange.
- Maternal changes:
- Increased appetite, less morning sickness, noticeable belly bump.
- Uterus expands and may cause pressure symptoms.
4. Third Trimester (Weeks 28–Birth)
- Key events:
- Fetal brain development accelerates.
- Fat layer builds for temperature regulation after birth.
- Lungs mature; surfactant production begins to prevent collapse after birth.
- Fetal position shifts — usually head-down (cephalic presentation).
- Fetal size: By week 40, average weight is 3–3.5 kg, length around 50 cm.
- Maternal changes:
- Shortness of breath due to upward pressure on the diaphragm.
- Back pain and swelling (edema).
- Braxton Hicks contractions (“false labor”).
5. Birth Process (Parturition)
- Hormonal trigger:
- Drop in progesterone.
- Increase in oxytocin from the pituitary gland — stimulates uterine contractions.
- Prostaglandins from placenta soften cervix.
- Stages of labor:
- Dilation Stage: Cervix opens up to 10 cm; amniotic sac may rupture.
- Expulsion Stage: Baby is pushed out through the birth canal.
- Placental Stage: Placenta is delivered after the baby.
- Newborn Adaptations:
- Lungs expand for first breath.
- Blood circulation changes — foramen ovale and ductus arteriosus close.


NCERT पुस्तकें – JEE और NEET तैयारी की पवित्र ग्रंथ | महत्व और रणनीति
जानें क्यों NCERT पुस्तकों को JEE और NEET की “पवित्र ग्रंथ” कहा जाता है। इनके महत्व, परीक्षा में सीधे प्रश्न आने की वजह, और सफलता के लिए NCERT को मास्टर करने की सर्वश्रेष्ठ रणनीति के बारे में पढ़ें।
Keep readingNCERT Books – The Holy Book for JEE & NEET Preparation | Importance & Strategy
Discover why NCERT books are called the “Holy Book” for JEE and NEET. Learn their importance, direct exam relevance, and the best strategy to master NCERT for success in competitive exams.
Keep readingClass 12 Biology Chapter 1 – Sexual Reproduction in Flowering Plants Notes PDF (Free Download)
Best Class 12 Biology Chapter 1 – Sexual Reproduction in Flowering Plants notes, covering every topic from flower structure to apomixis and polyembryony. Free, detailed, and easy-to-understand resource for CBSE Board and NEET preparation.
Keep readingComplete List of Biology Terms : Complete Glossary of Biology
Biology Glossary – Letter A Biology Glossary – Letter B Biology Glossary – Letter C Biology Glossary – Letter D 1. DNA (Deoxyribonucleic Acid) – Carries genetic instructions for development and functioning.डीएनए (डीऑक्सीराइबोन्यूक्लिक एसिड) – यह जीवों के विकास और कार्य के लिए आनुवंशिक निर्देश प्रदान करता है। 2. Diffusion – Movement of molecules from…
Keep reading



Leave a comment